Tips from #DData 2024 panelists, Dr. Albert Tzeel and Patty Telgener
The Payer Reimbursement Triad

1) Coding:
Coding is the standard mechanism for identifying a medical device. It involves assigning alphanumeric codes to the medical device, service, or procedure and its intended use in treatment. CPT codes are required for public and private insurance coverage of devices and treatments in the U.S.
Table 1: General Types of Codes
| Code | Description / Focus | Maintained by |
|---|---|---|
| HCPCS (Healthcare Common Procedure Coding System) | Entire coding system (Levels I & II) | Centers for Medicare & Medicaid Services (CMS) |
| CPT (Current Procedural Terminology) | Code set within HCPCS Level I used for medical services and procedures | American Medical Association (AMA) |
| HCPCS Level II | Code set within HCPCS but separate from CPT used for medical devices, supplies, DME, and other services | Centers for Medicare & Medicaid Services (CMS) |
Considerations:
- Learning about existing codes and their potential application to your medical device takes time and effort. Consider partnering with the deciding body (e.g., the American Medical Society, Endocrine Society).
- Coding requires broad market acceptance; you need to demonstrate the adoption of your medical device outside of academic and research institutions.
- There may be new coding requirements for specific AI-powered solutions.
2) Coverage:
Coverage refers to the criteria for deciding whether a payer will share the financial responsibility for a medical device, service, or procedure. Coverage determination hinges on alignment with established treatment protocols or standards of care for the specific patient diagnosis and proven outcomes.
Table 2: Categories of Outcomes
| Outcome | Description | Examples |
|---|---|---|
| Economic | Financial consequences; total cost of care and benefits for stakeholders | Long-term cost savings, increased revenue potential, reduced workforce burden |
| Clinical | Impact on patient health and disease management; safety and effectiveness | Health outcomes (e.g., lower A1C), prevention of complications, decreased mortality |
| Operational | Impact on healthcare delivery systems; efficiency and resource utilization | Ease of distribution, enhanced data sharing and integration, reduced hospital admissions |
| Humanistic | Impact on patient well-being and quality of life beyond clinical measures | Ease of use, increased independence, sleep quality, enhanced social interactions |
Considerations:
- To be considered standard care, a medical device must have a high adoption rate and traction within the relevant patient population (e.g., a glucose meter commonly prescribed by endocrinologists to people with type 2 diabetes).
- When it comes to coverage, value creation (ROI) is key. ROI = clinical impact + cost savings.
- Payers often look to published research to determine what medical devices are “coming down the pipeline.”
- A smartwatch is not a medical device and does not qualify for coverage.
“You invent a product. You think it’s worth top-dollar because you put your heart and soul into it, but you better have stellar outcomes that justify a high price.”
— Dr. Albert Tzeel, Humana Florida
3) Payment:
The third component of the Payer Reimbursement Triad is the payment level or dollar amount a payer agrees to contribute towards the cost of a properly coded and covered medical device, service, or procedure.
Considerations:
- You must be able to tell a story. Payers need to understand the impact of your medical device (outcomes), how much you intend to charge for your device, and why the cost is justified.
- Payers are fearful of high upfront costs and low utilization rates.
- Face-to-face meetings with payers are increasingly uncommon. Expect to complete online applications and submit a technology binder.
It’s never too early to start thinking about or planning for reimbursement.
Companies should integrate reimbursement considerations into their planning from the outset, ideally during the product development and clinical development phases. By incorporating reimbursement endpoints early on, companies can ensure that their reimbursement strategy is well-established and ready for implementation at the time of market launch.
#DData2024 Session TAKEAWAYS:
“It’s complicated”
“Show me the value” (outcomes + cost savings)
“It’s never too early to start”
ADDITIONAL LEARNINGS
Click HERE for a set of additional informative slides on Medical Device Reimbursement Strategies
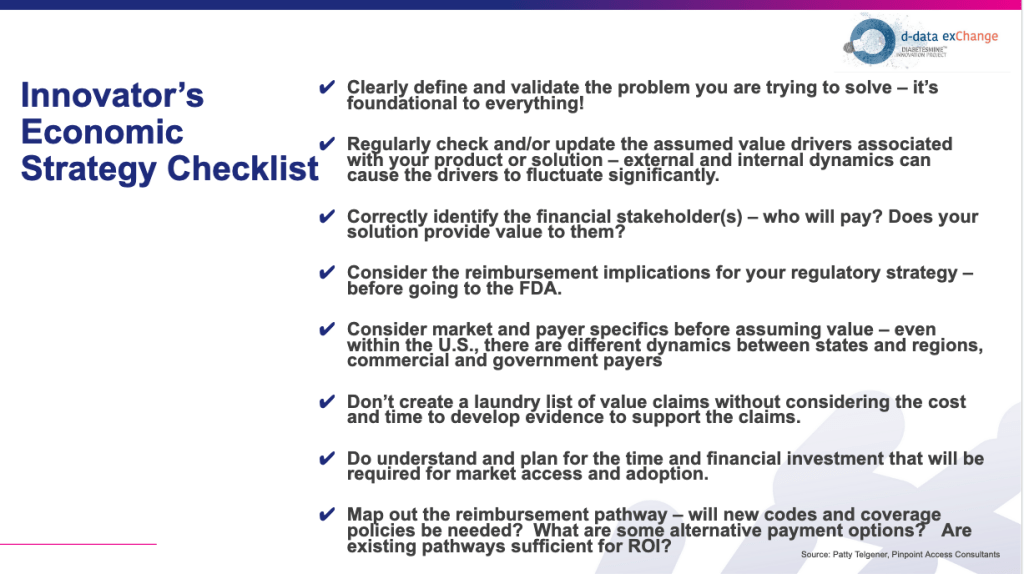
— Courtesy of Patty Telgener, Pinpoint Access Consultants